Plantar Fasciitis – Our arch enemy
Plantar fasciitis may sound like a new gardening fad, rather than the straining of the ‘plantar fascia’, or put in simple terms the band (fascia) of the foot (plantar). Known as ‘joggers heel’ because of the high incidence of this condition in those that run, plantar fasciitis is also the most common cause of arch pain.
With over ten percent of the population experiencing this condition in their lifetime, it is worth noting the causes and simple treatment that can prevent complications and avoid a longer term injury.
The feet and their relationship to the plantar fascia
Feet support the entire weight of the body during all upright activities, but unless they are injured their importance can easily go unnoticed.
With a quarter of all bones in the body situated in the feet, these complex extremities of the leg are held together by nearly twenty muscles and tendons as well as over a hundred ligaments. Over thirty joints allow the foot to move in a variety of ways, with the arch of the foot providing shock absorption through receiving and distributing the weight of body during activity.
Muscles, tendons and ligaments of the foot, and almost half the bones, form a flexible arch with which to absorb the pressure applied by body weight and motion. The arch is tensioned, much like a triangular truss, by a thick, flat, web like band of connective tissue known as the plantar fascia. Lying just beneath the skin on the sole of the foot, this band of three components connects the heel bone at one end of the triangle base, to the metatarsal bones at the other.
Serving as a clever function of the foot, this triangular truss incorporates the windlass mechanism, named after the windlass on a ship used to raise or lower an anchor. It involves firstly the rising of the foots arch, with simultaneous tightening of the foot and compacting of bones, as a step forward is taken. This then allows the foot to act as a shock absorber when the heel subsequently hits the ground, at which point it switches to a rigid lever to help drive the body forward to the next step.
Secondly the plantar fascia’s elastic properties provide further support by acting as a spring. As the foot makes contact with the ground, these soft tissues spread the contact reaction forces over a longer time span, helping to reduce forces upon the body.
This flattening of the arch and stretching of the plantar fascia also saves the body effort, as the soft tissue of the foot has the ability to temporarily store energy as it flattens. This energy is then released when the foot arches and the body is propelled forward, much like the elastic properties of a spring. When healthy, the components of the feet and the windlass mechanism, work without conscious effort.
Proper functioning of these structural and spring like mechanisms provides stability and efficiency for walking, running, jumping and any other activities involving the feet. Yet when these automatic movements are impaired, it is more than just the efficiency of the feet that is affected.
How does plantar fasciitis arise?
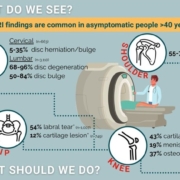
The plantar fascia’s major role of stretch and support in the function of the foot, and bearing some weight of the body, leaves it susceptible to injury. Stress upon this web like ligament can result in a condition known as ‘plantar fasciitis’. This is where the plantar fascia ligament is flexing beyond its normal range of motion, causing inflammation from which small tears in the tissue may result.
Pain will then be experienced in the arch or the heel of the foot, with heel spurs potentially developing in conjunction with plantar fasciitis. These are hard calcium deposits produced by the body in an effort to assist stability of the plantar fascia ligament.
As far as physical factors that can can increase the likelihood of developing this condition, high arched feet are less able to absorb impact, and cause extra strain to the fascia. Overpronation or the excessive inward turn of the foot, commonly known as flat feet, is also a common cause of pain of the arch and heal.
The effects of these physical attributes can be overcome with some forward thinking, and there are also some proactive measures to keep the plantar fascia happy.
What to consider in looking after the plantar fascia
Firstly arch support and heel cushioning is crucial and this can be achieved by wearing comfortable shoes that fit well. Ideally a shoe has support to lift and cushion the arch, along with a deep heel cup, to cradle the heel and absorb shock. Where a shoe fits most of these criteria, but lacks arch support or heel cushioning, a good quality shoe inserts can be added. Be sure to have an assessment or ask your physiotherapist if unsure as to what level of support will fit your needs.
Prolonged periods of standing can create a cumulative effect on the arch of the foot, especially if previously accustomed to a more sedentary lifestyle. This is due to strain being placed on a few muscles over a long period of time, rather than spread over numerous muscles. Standing on a hard surface such as concrete will add to the strain, so if unable to move about then a cushioned mat will offer some respite.
For exercise this is even more crucial as the impact feet absorb when running can be as much as four times a person’s bodyweight. Once again training on a surface that is harder than normal will exacerbate the effects of this impact. Sudden stretching or overuse of the sole during exercise, such as sprinting with poor technique off the blocks, running a distance that is greater than normal or an increased intensity in a workout session should be taken into consideration.
Should at any stage the achilles tendon become tight, this can affect the ability to flex the ankle, increasing the risk of injury to the plantar fascia. Also anything that effects the windlass mechanism described earlier can effect gait timing and the effectiveness of the body’s overall mechanics. Early intervention in this case can avoid putting undue repetitive stress on the fascia.
There are also some lifestyle factors to consider that can contribute to the onset of plantar fasciitis. Being overweight will place extra strain on your heel, as can the weight gain from pregnancy. Swelling of the feet is also experienced during pregnancy, causing ligaments to become relaxed, so extra care should be taken. Age can see a loss of elasticity in the foot and arthritis can cause inflammation, both of which are contributors to plantar fasciitis.
Thankfully in most cases, this condition can be resolved with some simple techniques, thus avoiding any future need for medication or surgery.
Treatment options for plantar fasciitis
A very high percentage of of cases involving plantar fasciitis resolve themselves, and in most cases can be treated without invasive and expensive treatment. If you feel heel or arch pain after exercise then follow the simple PRICE principle of protecting the area, resting the feet, applying ice for 15-20 minutes every two to three hours, compression with an elastic bandage and elevation by raising the foot above the level of the heart.
In some cases of more severe injury to the plantar fascia, anti-inflammatory medication may help pain and swelling. Keep in mind that this is best avoided in the first few days after injury as it may encourage additional bleeding.
Once the inflammation has had time to subside, the aim is to restore proper function to the foot. Central to this will be investigating the root cause and identifying the best course of action. A professional consultation such as physiotherapy, will be able to address these causes with treatment along with the prescription of stretching and strengthening exercises, specific to an individual’s condition. Hands on treatment can involve joint mobilisations, massage and dry needling. In some cases taping of the foot may be required or the wearing of a support, such as a plantar fascia brace or heel cups.
All of these will be in an an effort to protect the plantar fascia, and avoid further inflammation, while it heals. This may take anywhere from a weeks to months, in which time exercise and treatment can restore a full range of motion to the foot. Once achieved, stability can be restored through exercises that help regain muscle control of the foot arch. This can be in conjunction with the prescription of calf and other leg muscle exercises, dependent on the course of action within the physiotherapy treatment plan.
Once range of motion and stability have returned the plantar fascia to normal function, ensuring good foot biomechanics and the return of the perfect engineering of the windlass mechanism, will place the rest of the body in good stead. At this stage preventive measures mentioned previously can be explored, and in some cases a custom made orthotic may be recommended.
Of course being at a stage of good physical health is the time to address any running, jumping and landing techniques to further safeguard against injury and improve performance. A physiotherapist can assist in a customised program for sport specific training, as they can for a return to work program.
For the most part, early intervention through treatment, protection and the use of preventative measures, especially suitable footwear, should resolve minor cases of plantar fasciitis. Regardless of whether you have experienced this condition, when next springing out of bed, spare a thought for that which will help carry you efficiently though another day.