When is Abnormal Normal? MRI and normal aging
When is abnormal normal? Reframing MRI abnormalities as a normal part of ageing
Adam G Culvenor , Marcella Ferraz Pazzinatto, Joshua J Heerey
British Journal of Sports Medicine, July 2021

Sports and exercise medicine clinicians often refer for diagnostic imaging to help direct clinical management. The use of musculoskeletal MRI has risen rapidly in recent decades, yet the clinical benefit of MRI is uncertain.1 Imaging is useful for the differential diagnosis of many health conditions, including possible red flags, however, there are growing concerns of potential harm from MRIs caused by clinicians misinterpreting results triggering unnecessary interventions escalating patient fear/distress. Evidence-based reporting and clinically relevant interpretation of MRIs is critical. Recognising the clinical significance of MRI findings is often a challenge given the substantial discordance that exists between structural pathology and symptoms.
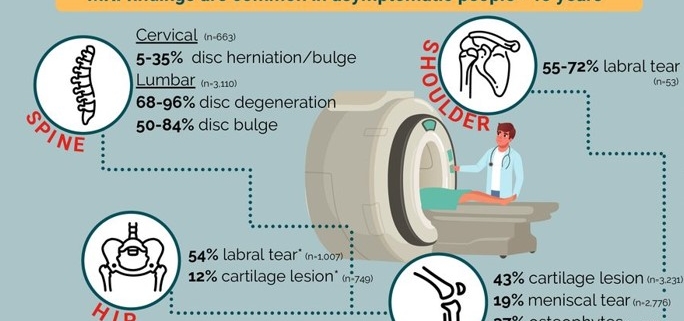
Emerging evidence indicates a high prevalence of so-called abnormal findings on MRI in individuals without symptoms. A collation of systematic reviews (and cohort studies when no review available) highlights that typical feature of deterioration, such as cartilage lesions, hip and shoulder labral tears and spinal changes (eg, disc degeneration/bulge) exist in many healthy asymptomatic adults (figure 1). Approximately 8 of 10 adults aged ≥40 years have asymptomatic disc degeneration, while almost half of all adults aged ≥40 years have knee cartilage lesions but no pain. Although the prognosis of these asymptomatic findings is not well established, even in cases of further structural deterioration (eg, longitudinal cartilage loss) the association with pain appears minimal.
These findings are critical for clinicians and patients to understand the relevance of structural pathology and can be used to address recent calls for radiology reports to include age-matched asymptomatic prevalence rates. Such an approach, together with discussion with patients putting MRI findings into context, may help minimise patient anxiety, and beliefs they are damaged and vulnerable, as a result of a diagnostic label. Including such epidemiological information on spinal MRI reports reduced subsequent opioid prescription although had little effect on healthcare utilisation.
The high prevalence of asymptomatic changes on MRI emphasises that such features may not always be the source of pain in symptomatic patients and should not routinely be considered as pathological processes requiring intervention. Instead, in many people they likely represent part of the normal ageing process— like wrinkles on the skin.
Current evidence suggests that it is more common than not to have a cartilage lesion or disc bulge as we age. Perhaps it is time we redefine what a ‘normal’ MRI is and start being CLEAR with patients when discussing imaging results—consistent language, including epidemiological information and assessment of relevance.